Background: Solitary fibrous tumors (SFT), formerly hemangiopericytomas, are rare, vascular, mesenchymal tumors with an aggressive biological phenotype capable of distant metastasis. Intracranial SFTs tend to be dural-based, localize to the skull base, parasagittal, or parafalcine regions, and are notoriously similar in appearance to meningiomas on imaging (although they only represent 2-3% of meningeal tumors). Gross total resection (GTR) of intracranial SFTs remains a challenge given their propensity for hemorrhage and frequent intimate involvement of critical neurovascular structures with reported surgical mortality as high as 9-24%. Furthermore, despite aggressive management with postoperative radiotherapy, recurrence rates are as high as 50-60% at 10 years. Stereotactic radiosurgery (SRS) is hypothesized to be particularly beneficial in the management of SFTs given their suspected inherent radiosensitivity from hypervascularity and the characteristic steep dose falloff gradient of SRS that allows for dose maximization while protecting adjacent structures. Published experience on SRS for SFTs, however, is still limited and an optimal SRS dosing strategy for successful local control without adverse effects remains unclear.
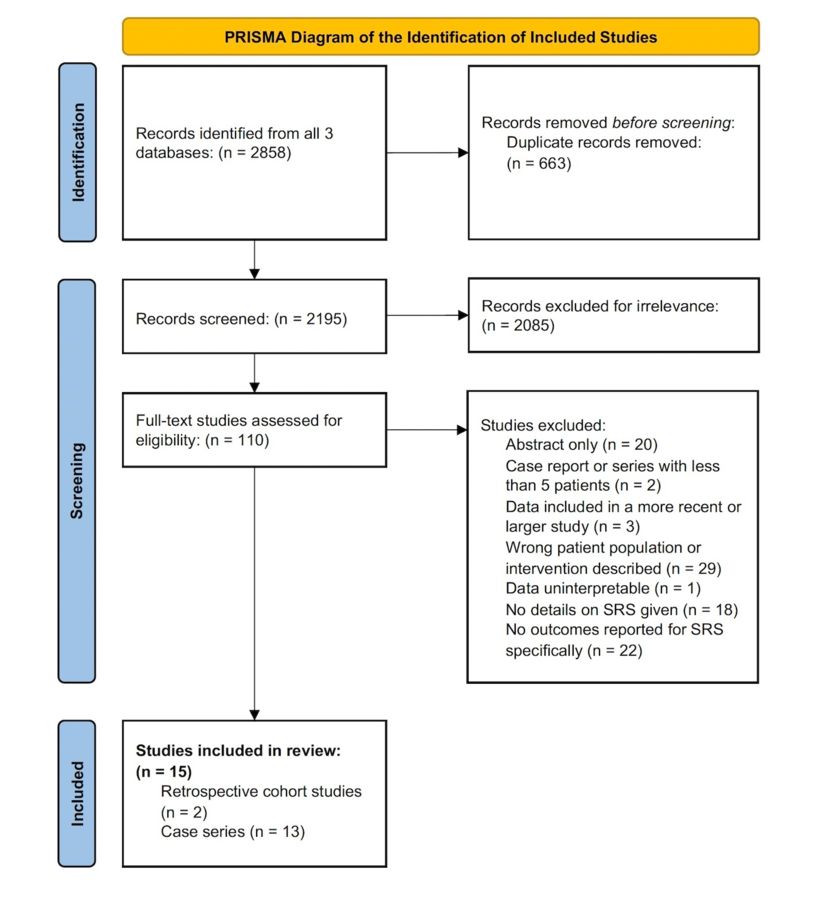
Methods: Following PRISMA guidelines, PubMed, EMBASE and Web of Science were systematically searched for all studies describing postoperative SRS for pathologically defined SFTs based on a predetermined search strategy described in the authors’ PROSPERO protocol (ID: CRD42023454258). Included studies described at least 5 patients, analyzed local tumor control as a primary outcome, and provided a mean or median SRS margin dose. Studies that gave SRS in more than 5 fractions or described data that was also included in another larger or more recent series were excluded.
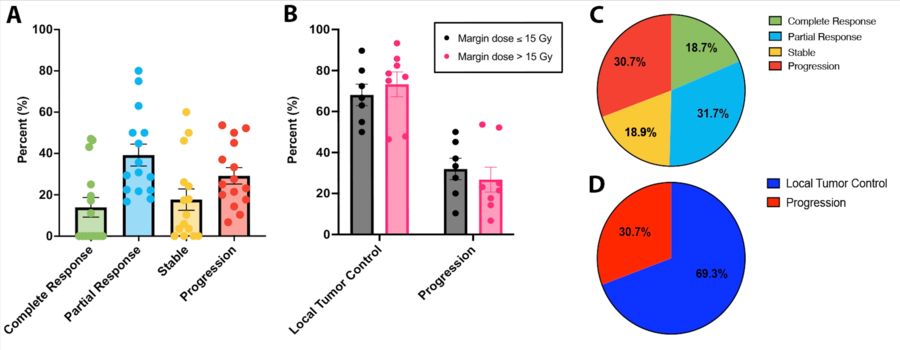
Results: Systematic review identified 15 studies for analysis (Figure 1), which yielded 293 patients and 476 intracranial residual or recurrent SFTs treated with SRS. Skull base SFTs represented 51% of the lesions treated. The treatment period spanned over 20 years (1987-2019). Patient age ranged from 13-80 years (mean 38-51 years), and most patients were male. At a mean follow-up of 21-77 months, overall local tumor control rate after SRS was 46.4-93% with a mean margin dose of 13.5-21.7Gy, mean maximum dose of 27-39.6Gy, and mean isodose at the 42.5-77% line. In pooled analysis, 18.7% of intracranial SFTs demonstrated a complete response to SRS, 31.7% had a partial response, 18.9% remained stable (overall local control rate of 69.3%, Figure 2D), and 30.7% progressed (Figures 2A and 2C). When stratified by margin dose, a mean margin dose >15 Gy showed a small benefit in local tumor control rate in pooled analysis (74.7% vs. 65.7%) (Figure 2B). There were only 4 symptomatic complications from SRS across studies (2 radiation necrosis, 2 radiation-related cavernous malformations with hemorrhage).
Conclusions: SRS is a safe and useful option for the postoperative management of SFTs with increasing margin dose likely providing improved local tumor control without significant adverse effects. Existing literature has focused on residual and recurrent SFTs, but our improved understanding of the aggressive biology of SFTs and the tolerated adjuvant SRS parameters could potentially be employed to develop an early postoperative adjuvant treatment paradigm, even after GTR.